Understanding SOAP Notes and the Role of AISOAP.com in Revolutionizing Medical Documentation
SOAP note, an acronym for Subjective, Objective, Assessment, and Plan, are one of the most widely used methods of documentation in healthcare. This structured approach to recording patient information has been a cornerstone of medical practice for decades. With the advent of artificial intelligence (AI), platforms like AISOAP.com are transforming how SOAP notes are created, offering healthcare providers a faster, more accurate, and efficient way to document patient encounters. Let's delve into the fundamentals of SOAP notes, their significance in healthcare, and how AISOAP.com is revolutionizing the process.
What Are SOAP Notes?
SOAP notes were first theorized by Dr. Lawrence Weed in the 1960s as part of the problem-oriented medical record (POMR) system. The format was designed to provide a structured framework for documenting patient encounters, ensuring that healthcare providers could systematically record and communicate critical information.
Components of SOAP Note
- Subjective (S): This section captures the patient’s perspective, including their symptoms, medical history, and personal experiences. It is often gathered through direct communication with the patient.
- Objective (O): This part includes measurable and observable data, such as vital signs, physical examination findings, and laboratory results. It provides an evidence-based foundation for clinical reasoning.
- Assessment (A): In this section, healthcare providers synthesize the subjective and objective data to arrive at a diagnosis or clinical impression. It reflects the clinician’s judgment and reasoning.
- Plan (P): The final component outlines the proposed treatment or management strategy, including medications, therapies, follow-up visits, and patient education.
The Importance of SOAP Note in Healthcare
1. Standardization and Consistency
SOAP note provide a standardized format that ensures consistency in documentation across healthcare settings. By adhering to this structured approach, healthcare providers can minimize variations in documentation style, enhancing the quality of patient records.
2. Facilitating Communication
SOAP notes serve as a communication tool among members of the healthcare team. The clear and organized format allows clinicians to easily share and review patient information, ensuring continuity of care across different specialties and care settings.
3. Legal and Ethical Compliance
Accurate and comprehensive SOAP notes fulfill legal and ethical obligations, providing a documented timeline of care that can be used in case of audits or legal disputes.
4. Cognitive Framework for Clinical Reasoning
The structured format of SOAP notes acts as a cognitive aid for clinicians, guiding them through the process of assessing, diagnosing, and treating patients. It ensures that no critical detail is overlooked.
Challenges in Traditional SOAP Note Documentation
Despite their benefits, traditional SOAP note documentation can be time-consuming and prone to errors. Healthcare providers often face the following challenges:
- Administrative Burden: Clinicians spend significant time on documentation, reducing the time available for direct patient care.
- Inconsistencies and Omissions: Human input can lead to inconsistencies or the omission of critical details, compromising the quality of patient records.
- Burnout: The repetitive nature of documentation contributes to clinician burnout, affecting their overall productivity and well-being.
How AISOAP.com is Revolutionizing SOAP Notes
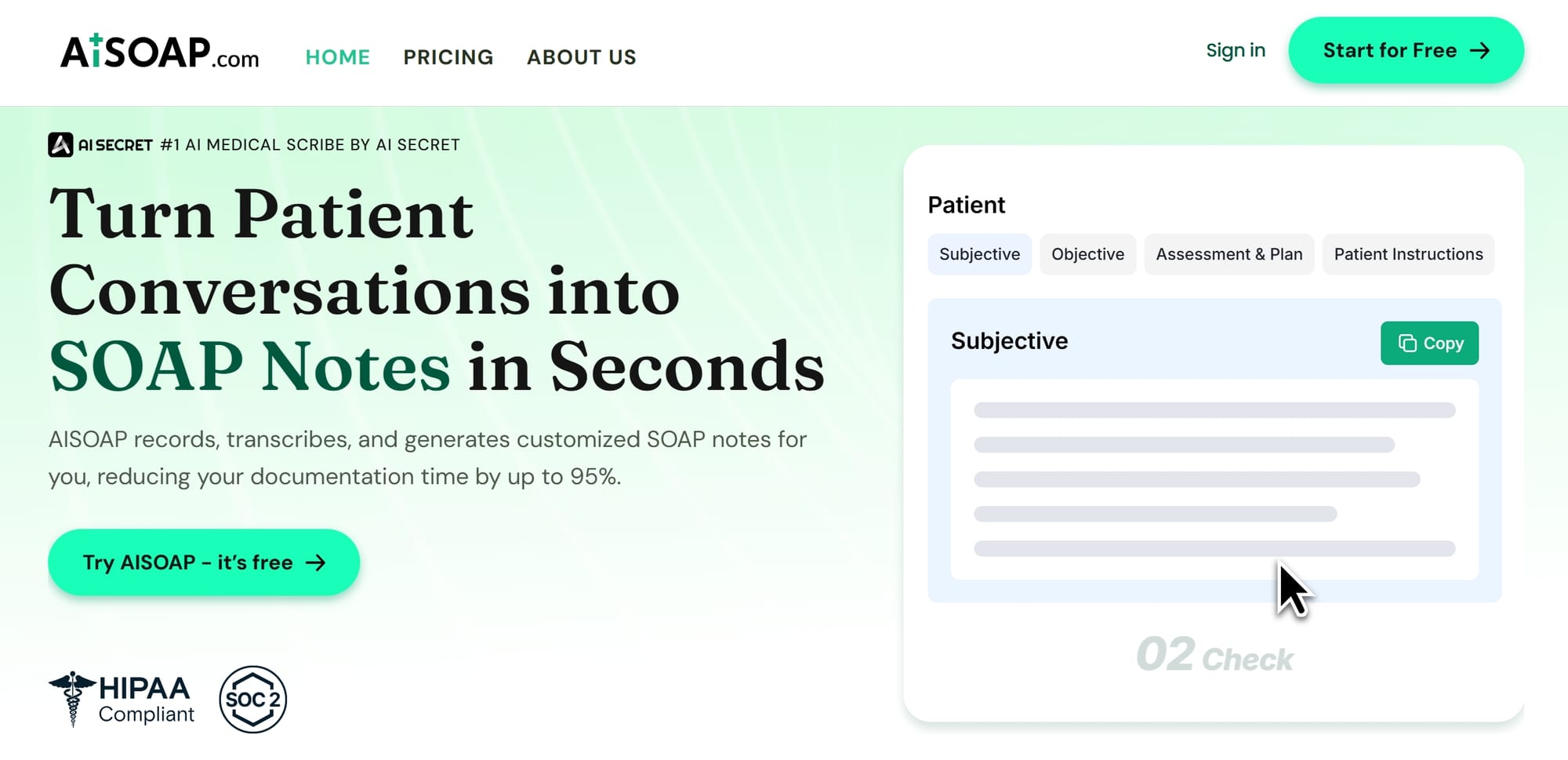
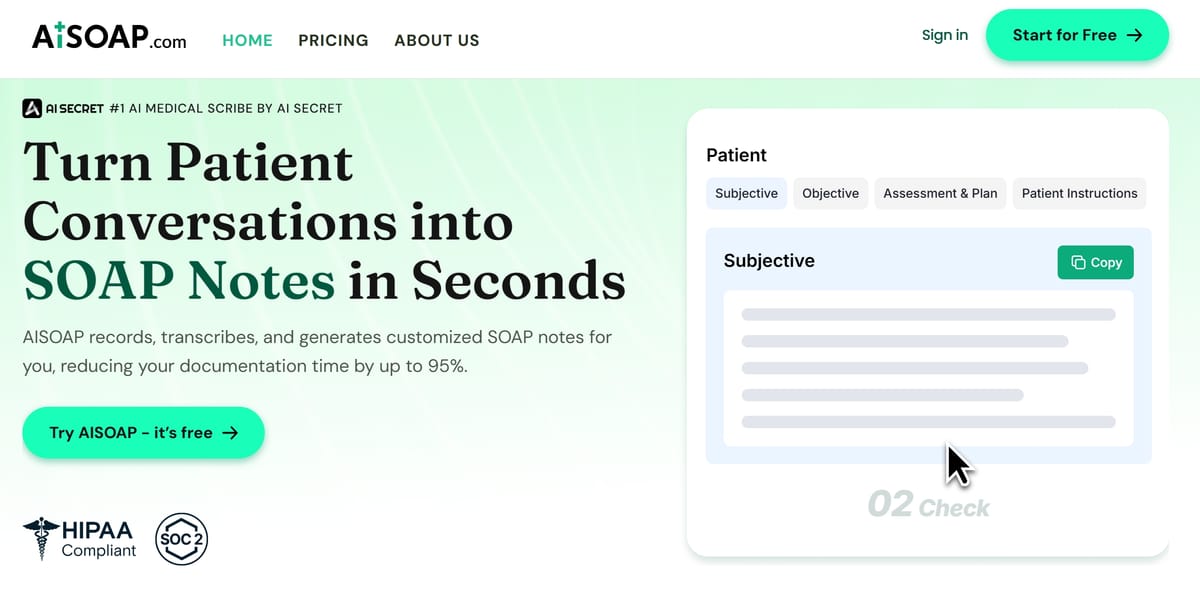
AISOAP.com is an AI-powered platform that addresses the challenges of traditional SOAP note documentation. It leverages cutting-edge technologies like natural language processing (NLP) and machine learning to automate and streamline the process. Here’s how AISOAP.com is transforming medical documentation:
1. Efficiency and Time Savings
AISOAP.com enables healthcare providers to generate detailed SOAP notes effortlessly from shorthand, dictation, or telehealth sessions. By automating the documentation process, clinicians can focus more on patient care and spend less time on administrative tasks.
2. Accuracy and Completeness
The platform ensures that all relevant details are captured, reducing the risk of errors and omissions. This improves the quality of patient records and enhances clinical decision-making.
3. Standardization and Consistency
By adhering to predefined templates and guidelines, AISOAP.com maintains uniformity in format and content. This consistency facilitates seamless communication and collaboration among healthcare providers.
4. Security and Privacy
AISOAP.com is fully HIPAA-compliant and SOC 2 certified, ensuring the confidentiality and integrity of patient data. The platform employs robust encryption and access controls to safeguard information against unauthorized access or disclosure.
5. Reducing Burnout
By minimizing manual entry and streamlining workflows, AISOAP.com helps alleviate the administrative burden on clinicians. This allows them to dedicate more time to patient care and reduces the risk of burnout.
Testimonials and Real-World Impact
Healthcare professionals who have adopted AISOAP.com report significant improvements in their workflow and productivity. For instance:
- Dr. Todd Carman-Wagner, Ph.D., DSW-LICSW, shared that AISOAP.com was particularly helpful during a busy clinic day, allowing him to quickly generate accurate SOAP notes and save time.
- Dr. Samara Toussaint, a psychologist, emphasized how the platform helped her complete timely notes and provided key insights for professional documentation.
These testimonials highlight the platform’s ability to enhance efficiency and improve the overall documentation experience for healthcare providers.
The Future of SOAP Notes with AI
As AI technology continues to evolve, platforms like AISOAP.com are poised to play an even more significant role in healthcare. By automating routine tasks, these tools empower clinicians to focus on what matters most—providing high-quality, compassionate care to their patients.
The integration of AI in SOAP note documentation represents a paradigm shift in medical practice, offering a glimpse into a future where technology and healthcare work hand in hand to improve patient outcomes.
SOAP notes remain an indispensable tool in healthcare, providing a structured framework for documenting patient encounters. However, traditional methods of documentation are often time-consuming and prone to errors. AISOAP.com addresses these challenges by leveraging AI to automate and streamline the process, offering healthcare providers a faster, more accurate, and efficient way to create SOAP notes. With its commitment to security, privacy, and user-friendly design, AISOAP.com is setting a new standard for medical documentation, ensuring that clinicians can focus on what truly matters—delivering exceptional patient care.